By: Aphrodite Kotrotsios, Publisher
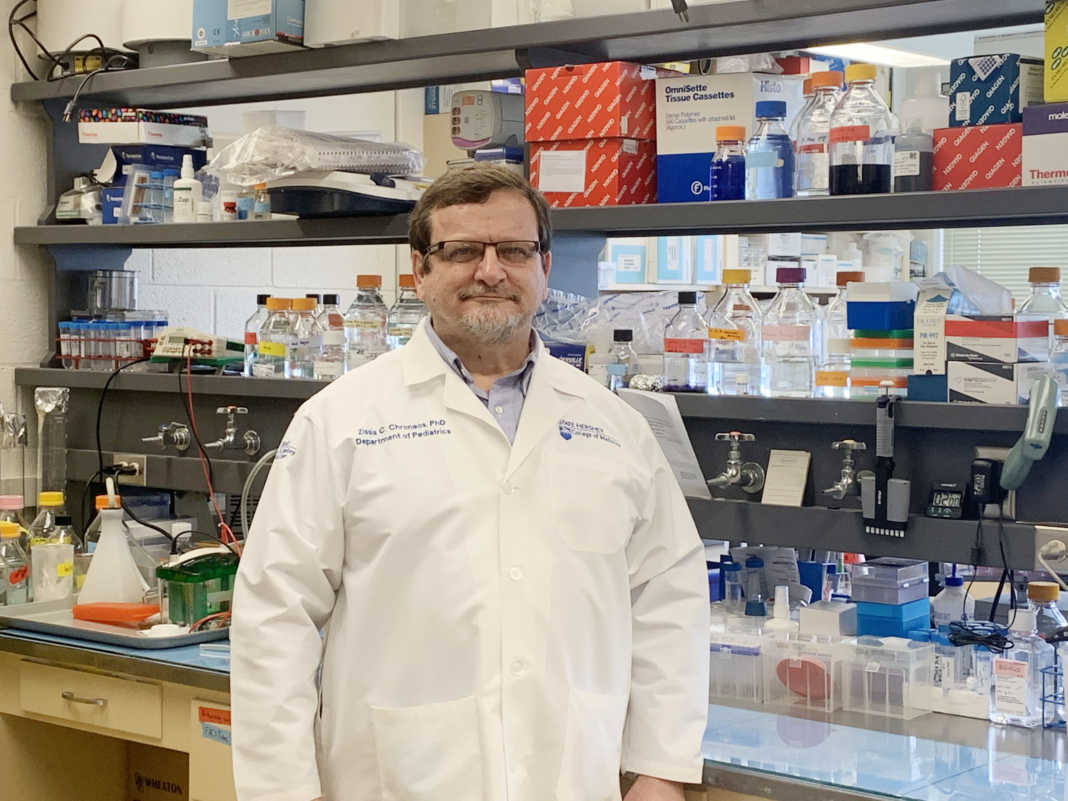
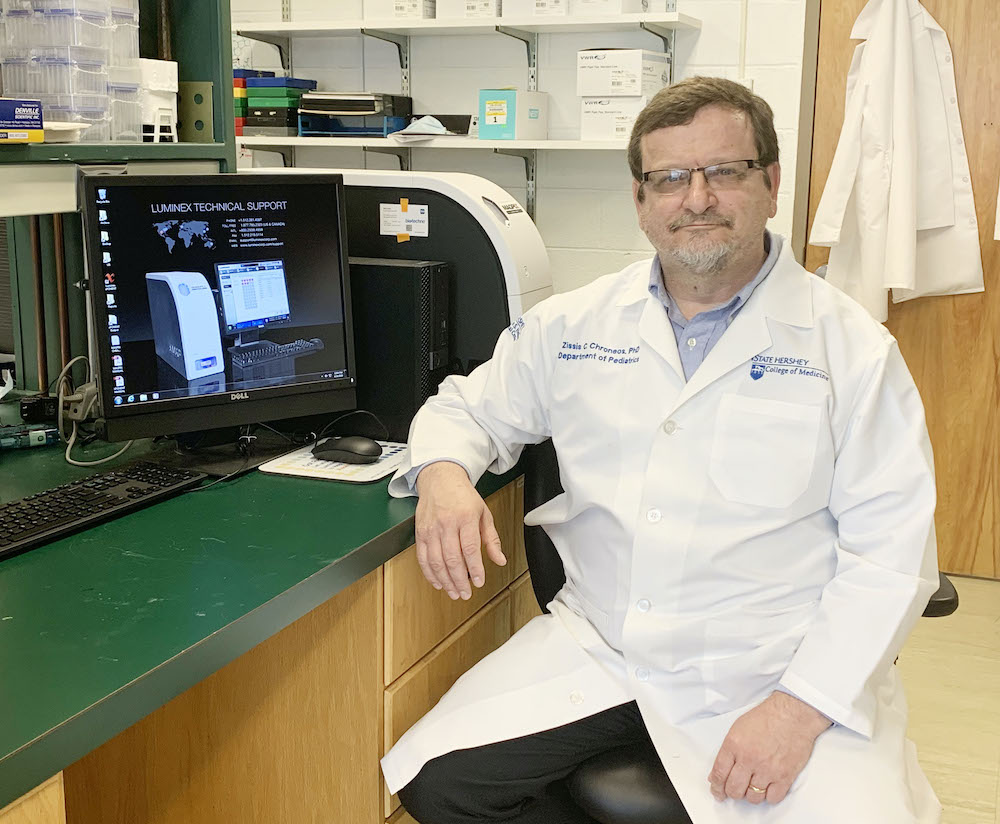
Dr. Zissis Chroneos is a Professor of Pediatrics, and Microbiology and Immunology at Pennsylvania State University (Penn State) College of Medicine, Hershey, PA since 2011. His main research focus at Penn State College of Medicine is on influenza pneumonia and treatment of influenza inflammatory disease, which kills hundreds of thousands to millions of people worldwide during seasonal epidemics and periodic pandemics. He is Co-Founder of Respana Therapeutics, Inc established in 2017. He holds American and International patents on therapeutics for the treatment of inflammatory syndromes. He immigrated to America in 1983 as soon as he graduated from high school in Evia, Greece. He earned a Doctoral (Ph.D.) Degree in Chemistry (1992) from the University of South Carolina, Columbia, SC, and Bachelor of Science (B.S.) degree in Biochemical and Biophysical Sciences (1998) from the University of Houston’s Honors College, Houston, TX. In 2019, he was appointed to AHEPA’s National Cooley’s Anemia Foundation Committee to help find cures and treatments for Cooley’s anemia, a severe form of β-Thalassemia of high genetic prevalence in individuals with Greek heritage. Here is what he had to say to the publisher of the Hellenic News of America, Aphrodite Kotrotsios on novel Coronavirus.
Aphrodite Kotrotsios (AK): Your research focuses on the pathogenesis of influenza. What can you tell us about COVID-19’s pathogenesis?
Dr. Zissis Chroneos (DZC): Coronavirus disease of 2019 abbreviated as COVID-19 describes the disease caused by a novel Coronavirus (CoV) named SARS-CoV-2, which was first reported in the Wuhan Province in China at the end of 2019. SARS-CoV-2 belongs to the genetically related severe acute respiratory syndrome-related Coronavirus family. A member of this family known as SARS-CoV caused a smaller pandemic in 2003. The designation COVID-19 has been adopted by the World Health Organization to distinguish the evolving spectrum of respiratory and systemic disease triggered by the etiologic agent SARS-CoV-2. Individuals who become infected with SARS-CoV-2 may remain asymptomatic, experience mild to severe symptoms, or progress to critical respiratory illness that requires hospitalization. Imaging of lungs by computed tomography also known as CT scan has revealed that COVID-19 disease is present even in the absence of overt symptoms.
Infected individuals spread the infection from person to person regardless of the presence of symptoms or disease severity and remain contagious as long as they carry live virus in their respiratory secretions for two to four weeks after infection onset and up to two weeks after resolution of clinical symptoms. The epithelial cells in the nasal cavity and throat are the first to become infected and produce respiratory secretions that eject virus in short and long-range aerosols in the form of large and small droplets, respectively. Transmission occurs primarily through direct contact such as a handshake, touching of the face and contaminated surfaces, but can also occur indirectly by inhalation of short and long-range aerosols.
SARS-CoV-2 gains entry in host cells by a two-step process, a binding step and an enzymatic step, that allows the virus to attach and release its genetic material into host cells, respectively. Attachment involves the binding of the spike protein that protrudes from the surface of the virus to the receptor angiotensin-
The heterogeneous manifestation of COVID-19 disease is thought to be related to differences in the levels of ACE2 across the respiratory tract and the vascular compartment of the lung, enzymes that can activate the fusogenic activity of the spike protein, the presence of comorbidities, and age of affected individuals. Immune senescence that occurs as a function of age may contribute to disease severity compared to children who present with only mild symptoms but are equally susceptible to infection as older individuals. Senescence represents an inflammatory state with limited capacity to develop immunity and eradicate infection.
The fitness of SARS-CoV-2 that allowed the transition from the pre-epidemic zoonotic phase to human to human transmission is related to genetic adaptations in the receptor-binding domain, protease cleavage sites, and modification of the spike protein with complex sugars. The respective impact of these adaptations are enhanced binding affinity to human ACE2, expanded repertoire of enzymes in human cells that can cleave and activate the fusogenic activity of the spike protein, and enhanced stability of the spike protein. Glycosylation changes may have altered the interaction of the virus with the immune system towards pathogenic immune responses that divert the virus to alternate routes of entry in inflammatory immune cells. Increased binding affinity to the human ACE2 receptor predicates that SARS-CoV2 has increased efficiency to infect epithelial cells with low expression of ACE2 in the nasal cavity, throat, and upper respiratory tract, and immune cells that come to the site of infection. The biological outcome of these events is successful establishment of the virus infectious cycle, and delayed development of immunity to eradicate the virus.
The virus can then spread to the alveolar sacs of the lung and avidly infect Alveolar type II epithelial cells, which express high levels of ACE2. Alveolar type II epithelial cells produce surfactant, a complex of lipids and proteins lining the alveolar surface. Surfactant is required for effortless breathing and to prevent fluid leakage from the lung’s capillaries into the alveolar space. The virus may penetrate deeper into lung tissue, cross the alveolar-capillary barrier, and infect ACE2 rich capillary endothelial cells. ACE2 regulates blood pressure responses in the blood circulation. Immune cells that rush to the lung to fight the infection plug the lung’s interstitial spaces and generate an excess of inflammatory mediators that alter the normal anatomical structure of the lung, preventing blood oxygenation and exhalation of excess carbon-dioxide. This compromised gas exchange results in a combination of respiratory dysfunctions that manifest clinically as hypoxia, hypercapnia, and dyspnea that deprive the body’s tissues of adequate oxygen supply, ability to regulate cardio-respiratory tone, and ability to maintain acid-base balance in the blood.
Acute lung and tissue injury from inflammatory and respiratory disruption is the end-stage manifestation of the disease with limited treatment options other than supportive and compassionate care and very poor prognosis for survival.
(AK): Can you explain a bit about the body’s innate immune response to viral infections and when is the adaptive immune response activated?
(DZC): The innate immune response encompasses physical, biochemical, chemical, and cellular barriers to infection. Physical barriers include mucous and the mucociliary escalator in the upper respiratory tract. Biochemical and chemical barriers include digestive enzymes, inhibitory proteins that prevent infection of epithelial cells, complement, bactericidal proteins, reactive oxygen radicals elicited in response to infection, interferons and inflammatory mediators elicited by immune and other cells in the presence of infection. Cellular barriers include a range of innate immune cells including macrophages, dendritic cells, monocytes, natural killer cells, neutrophils, mast cells, and innate lymphocytes that populate the lung constitutively in both airway and tissue compartments. Alveolar macrophages are the first line cellular defense patrolling alveolar spaces. They display an array of non-specific receptors that grab pathogens and deliver these to intracellular digestive vesicles called lysosomes without eliciting an inordinate amount of inflammatory mediators but transmit sufficient signal to alert the adaptive immune system to entry of new pathogens. These include scavenger receptors, lectin receptors, toll-like receptors on the macrophage surface, and intracellular recognition systems that detect the presence of proteins and genetic material of viral proteins. This critical property occurs in conjunction with surfactant proteins that maintain alveolar macrophages in an anti-inflammatory but immune vigilant state to respond quickly to external threats. Alveolar macrophages emit signals that activate other innate immune cells to secrete antiviral substances and work together to elicit activation of the adaptive immune system.
Pathogens that breach this barrier through immune evasion mechanisms suppress innate immune recognition allowing the offending pathogen to proliferate to high levels and damage the lungs before detection by the adaptive immune system. At this stage, the combination of tissue damage and infection amplify the immune response that may eradicate the virus but the inflammation is difficult to resolve inflicting persistent tissue damage and prolonged rounds of inflammatory cycles.
The adaptive immune system contains cellular and humoral branches that eradicate infection, control inflammation and generate memory responses that establish short-term (ie months to years) to life-long protective immunity. Protective immunity can wane over-time depending on the antigenic repertoire processed for different pathogens at the early stages of infection. The cellular branch of the adaptive immune system includes T and B lymphocytes. T lymphocytes process antigen, kill infected cells, secrete interferons that suppress viral proliferation, and differentiate to memory T cells, and help B cells to secrete antibodies among many other functions. B lymphocytes process both non-protein and protein antigen and maintain the humoral immune system though life-long secretion of antibodies. Antibodies bind pathogens mediating clearance by macrophages and activate the classical complement cascade to kill pathogens.
Clearance and eradication of SARS-CoV2 appears to depend on humoral immunity. That is, the production of antibodies. The production of antibodies against SARS-CoV-2 coincides with the reduction of viral load in asymptomatic and mildly ill individuals and resolution of symptoms if any. The development of anti-SARS-CoV-2 antibodies in these individuals takes about 3 weeks. During this period, they can shed the virus to the community. Individuals who develop severe symptoms and subsequently recover can continue to shed virus for 1-2 weeks during recovery from COVID-19. The reasons for this presentation are not yet clear. It has been found that some patients with COVID19 develop pathogenic antibodies that amplify inflammatory responses by delivering infection in immune cells in which degradation of the virus is incomplete. Viral fragments can trigger excessive inflammation by the innate immune system or alternatively, allow some virus to escape, proliferate, and deplete immune cells. It takes additional time for those who develop partial inflammatory immunity to produce additional antibodies or cell-mediated responses to eradicate the virus. The levels of antiviral immunity and its impact on individuals who develop critical COVID-19 illness is not yet known.
(AK): What makes this particular Coronavirus strain significantly concerning?
(DZC): SARS-CoV-2 is a highly contagious strain with mixed-mode of contact and airborne transmission. It can shed into the feces increasing the risk for fecal and fecal-oral transmission in poor hygienic conditions, although it is not yet established whether this transmission route contributes to widespread infection. SARS-CoV-2 has a prolonged incubation period lasting for up to three weeks after infection that allows unsuspecting individuals to spread the infection in the community. The reasons for this are not yet understood. One possibility is that partial pre-existing immunity to related Coronavirus strains sustains a tolerable level of transmissible virus that may delay the development of specific immunity to this particular strain. This late onset immune response may help clear the virus but also generate adverse inflammatory reactions that can range from mild to critical. The possibility of co-infection with other respiratory viruses or bacteria causing superinfection has not been adequately addressed. The epidemiological curves in severely affected areas exhibit a prolonged peak period followed by a slow decline for both new cases and fatalities suggesting overlapping waves of infection, partial compliance to mitigation directives and/or infection of index cases with sub-strains of SARS-CoV-2. This may prolong the persistence of the pandemic limiting efforts to return to normalcy.
(AK): To date, what do we know about this virus?
(DZC): SARS-Cov-2 is the third member of the beta CoV family to cause a pandemic in the past 25 years, and the first to cause a rapid widespread pandemic from human to human transmission. SARS-Cov-2 also infects cats and ferrets. The molecular coordinates and amino acid adaptations that enabled the penetrance of SARS-Cov-2 in the human population have been mapped by both molecular modeling and experimental levels. SARS-Cov-2 originated as a zoonotic infection from bats through an intermediate species. Bats are the main natural reservoir of different Coronavirus species. Molecular evidence indicates pangolins as the putative intermediate species. The spike protein of SARS-CoV-2 may exhibit molecular promiscuity in that it can utilize several receptors that may allow it to enter cells that do not express the main receptor ACE2.
SARS-CoV-2 is an enveloped ribonucleic acid (RNA) beta Coronavirus of the genetically diverse Orthocoronoviririnae family that circulate in many avian and mammalian species. The CoV envelope displays the spike proteins that attaches the virus to host cells and other proteins that are required to promote the propagation and release of virus progeny from host cells. The envelope encloses a capsid that contains the RNA genetic material. The CoV RNA is among the largest known ranging between 25 to 32 kbases. Coronaviruses are also the largest viruses known with diameters ranging 0.1-0.13 nanometers in diameter. The Orthocoronoviririnae family is taxonomically categorized into 4 genera: alpha, beta, gamma, and delta. Alpha and beta Coronaviruses infect mammals, gamma Coronaviruses infect avian species, and delta Coronaviruses infect both mammals and avian species.
(AK): What are the alarming symptoms that people should look for?
(DZC): Persistent low-grade fever requires monitoring and follow-up, fatigue, persistent low-grade headaches
(AK): How can we overcome the challenges we are facing from this pandemic?
(DZC): Adherence to public health measures to contain the pandemic, save lives, and develop countermeasures to mitigate the pandemic in a diverse but a resourceful democratic society is a major and unprecedented challenge to the character of the Nation. From the scientific perspective, understanding the epidemiological patterns of both COVID-19 disease and interstate spread of the virus in the US population compared to the rest of the world is critical to dynamically adjust public health approaches to containment, mitigation, preventive follow up, inform research efforts and point of care medical intervention, and cautious return to normalcy. We have the means to accomplish this through testing and assessment of viral spread and mutation by sophisticated sequencing and molecular technologies that can provide rapid information about the virus in multiple academic, federal, pharmaceutical, and health care organizations throughout the country. We can predict the pathogenicity of SARS-CoV-2 sub-strains by molecular modeling and validate computational data experimentally relatively quickly. The same approach is being used to identify potential drugs to treat the infection but this is needed at a much larger scale than current efforts. Investment, communication, and cooperation at both the national and international levels are critical components of success.
(AK): How long do you think it will take before there will be a vaccine for COVID-19 and antivirals?
(DZC): The current prediction is 12-18 months, but this estimate is predicated on the assumption that a vaccine candidate with favorable safety profile can be produced, stockpiled, and distributed rapidly to health care organizations within this time period. At this point in time, several vaccine candidates have likely shown efficacy in preclinical testing. Most vaccines are designed to generate antibodies against the virus. One unknown at the moment is whether the vaccines elicit an antibody profile that eradicates the virus without enhancing pathogenic inflammatory reactions. That is, whether a given vaccine is safe or not.
The prospect for antiviral and host targeted drugs to ameliorate inflammatory symptoms may come into play in less than a year and we need to have multiple to treat the heterogeneous disease of COVID-19. One of the antivirals Remdesivir in current use for compassionate care has shown some efficacy and may be in wider use soon. Hydroxychloroquine and Zithromax have an interesting mechanism of action rationale but at this point in time, there is no agreement as to whether they are helpful without data from randomized control trials. Hydroxychloroquine is counter-indicated for individuals with G6PD deficiency and other more rare blood disorders, which is common in individuals with Mediterranean and Asian heritage. They will likely be helpful to some patients for the treatment of associated co-morbidities. There are new drugs that have shown promise in preclinical trials that have not gone through approval for clinical use yet.
Immunotherapeutics that block inflammatory pathways, transfer of convalescent serum, and cell therapies with mesenchymal stem cells are additional approaches that show promise in either preclinical or clinical stages. Of these, transfer of convalescent serum would have the most immediate impact if it works.
(AK): Why is it important that people do not self-medicate?
(DZC): Medications carry side effects that manifest differently in different individuals. They should not be taken without medical supervision.
(AK): What can we do from our homes to stay healthy?
(DZC): My wife is working from home and three of my kids are home taking their courses online. They have been home since before the outbreak started to take hold in our area, so social distancing is less of an issue. I still work from my office at work at Penn State College of Medicine, although the building where my office is now pretty much deserted and physically separated from the hospital and patient traffic. At home, we observe the standard precautions to wash hands and clean hands, surfaces, and clothing thoroughly, observe an exercise routine, eat healthy, sleep well and support each other and have adhered to the lent schedule to the extent possible. We communicate frequently with my fourth daughter who is working from home in Washington, D.C. We communicate frequently with friends and relatives through Skype and social media. We visit the grocery and other stores infrequently. Most standard items and food we order online.
(AK): How has this crisis changed you as a person, as far as your view of your life and your career?
(DZC): I had to slow down research activities in the lab and retool to deliver all medical and graduate school classes and meetings via zoom. I maintain regular communication with colleagues and staff outside “zoom hours”. As principal investigator of a biomedical research laboratory, the sense of responsibility and gravity that this position entails have reached a new level of urgency. I am personally affected. One of the investigators in my lab is recovering from COVID-19. He acquired the infection from a household contact who became ill from the disease from infection in the workplace. Clinical colleagues in the lab are among those who take care of COVID-19 patients. I have remained in contact with my former trainees in New York and Wuhan, China during the pandemic who have served in the frontline taking care of COVID-19 patients. I am very proud of them and wish them and their families well. As far as my career is concerned, I am adopting COVID-19 related research in my laboratory.