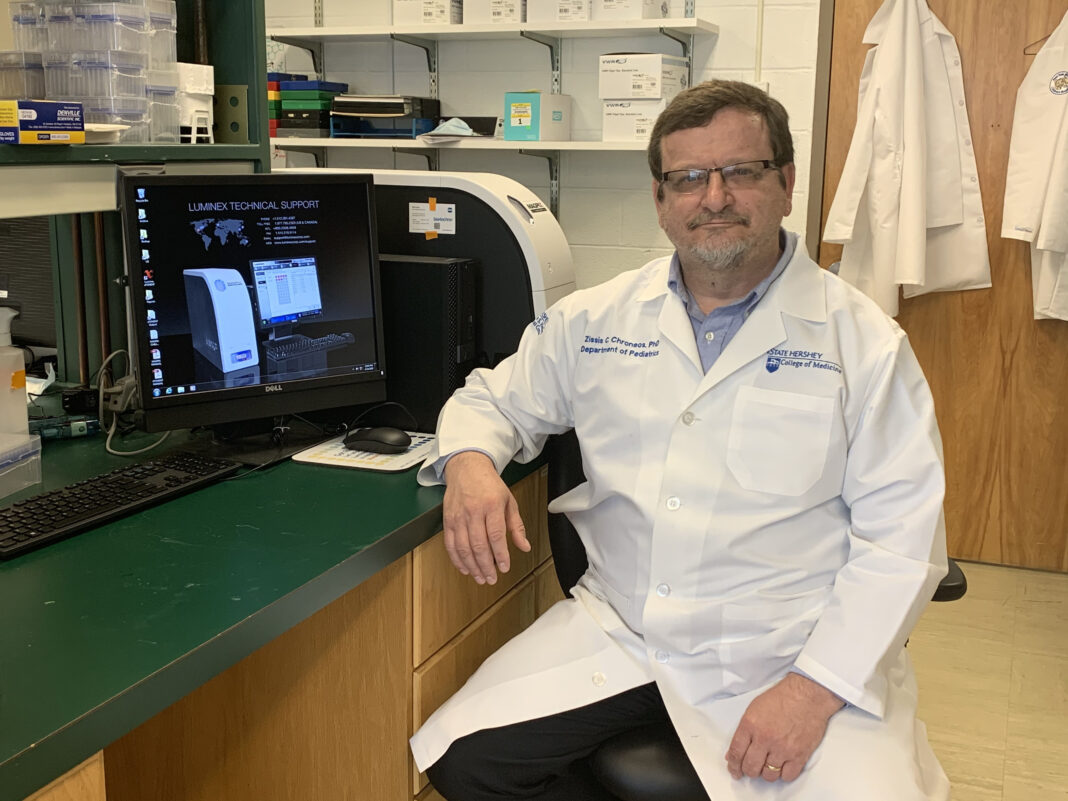
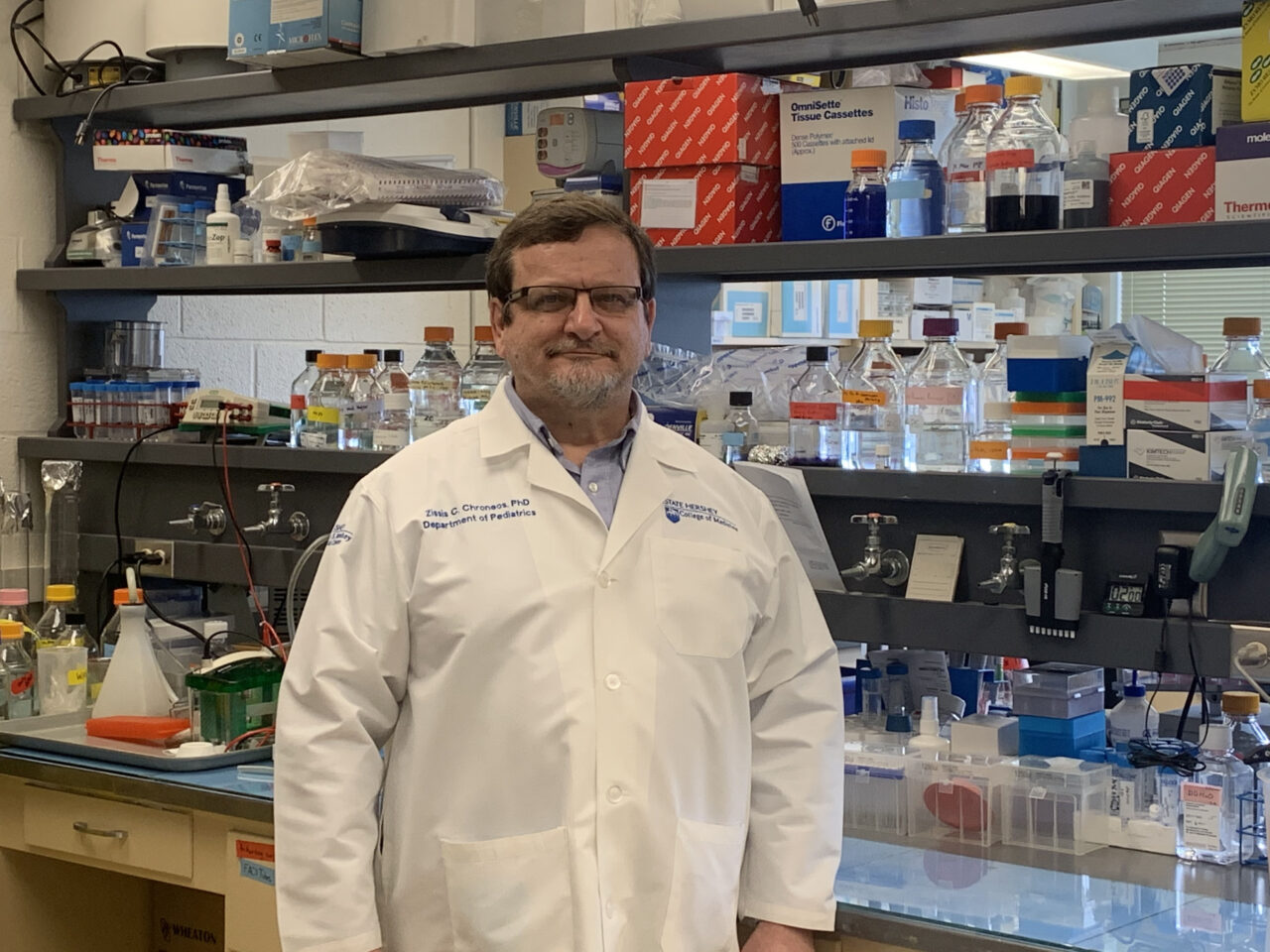
Dr. Zissis Chroneos chatted with Aphrodite Kotrotsios, the publisher of the Hellenic News of America, in order to provide a better understanding of the COVID-19 vaccines. Dr. Zissis Chroneos is a Professor of Pediatrics, and Microbiology and Immunology at Pennsylvania State University (Penn State) College of Medicine, Hershey, Pennsylvania, since 2011. His main research focus at Penn State College of Medicine is on influenza pneumonia and treatment of influenza inflammatory disease, which kills hundreds of thousands to millions of people worldwide during seasonal epidemics and periodic pandemics. He is the co-founder of Respana Therapeutics, Inc., which was established in 2017. We hope that this interview will better educate the public on COVID-19 vaccines and help them in making the right decision for their health. Here is what Dr. Chroneos had to say.
AK: How many new vaccines are on the horizon?
DZC: As of February 12, 2021, there are 242 vaccine candidates under development throughout the world (https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines). Of these, 66 have advanced to clinical development in phase 1 to phase 3 randomized controlled clinical trial stages while 176 are in pre-clinical development stages. The primary goal of vaccines is to elicit the production of high affinity neutralizing antibodies that can bind antigens on the virus and thus block the ability of the live virus to infect and cause disease. The most common vaccine types in clinical development and beyond include protein subunit vaccines, non-replicating viral vector DNA vaccines, and liposome encapsulated mRNA vaccines. Protein subunit vaccines utilize one or more protein antigens sourced from the virus in combination with an adjuvant. The viral vector DNA vaccines utilize live but non-replicating adenovirus that can enter target cells and encode a coronavirus protein antigen through transcription and translation of a coronavirus DNA gene. The mRNA encapsulated liposome based vaccines are taken up by immune cells wherein the host cell translates the mRNA into a coronavirus protein. Most of these vaccine platforms present the coronavirus spike protein S that is highly immunogenic and aptly recognized by the immune system as an antigen to produce neutralizing antibodies. More traditional vaccine approaches that utilize inactivated or attenuated forms of the virus have also reached the clinical development stage.
Five vaccine frontrunners have already received emergency use authorization in one or more countries having demonstrated 90-95% vaccine efficacy in randomized control phase 3 clinical trials. Vaccine efficacy entails percent reduction in disease incidence in a vaccinated group compared to an unvaccinated group receiving a placebo. The frontrunners include two mRNA vaccines from BioNTech/Pfizer (Germany/US) and Moderna (US), two non-replicating adenovirus vector based DNA vaccines from The University of Oxford/AstraZeneca (UK) and The University of Beijing/CanSino Biologics (China), and a heterologous non-replicating adenovirus vector based DNA vaccine from The Gamaleya Natural Center of Epidemiology and Microbiology (Russia). The BioNTech/Pfizer BNT162b2, Moderna mRNA-1273, and The University of Oxford/AstraZeneca AZD1222 vaccines have been approved by the World Health Organization for international use. The CanSino Biologics Ad5-nCOV and the Gamaleya Sputnik V vaccines received early authorization last summer following completion of phase 2 safety studies in China and Russia, respectively. Both are awaiting international approval later this year upon completion of phase 3 efficacy studies later this year. Only two, the BioNTech/Pfizer and Moderna mRNA vaccines are currently approved in the USA.
In the near term, there are three vaccines that are or expected to undergo regulatory review for approval by mid-summer. An adenovirus vector based DNA vaccine from Janssen/Johnson&Johnson (The Netherlands/US) designated as Ad26.COV2.S is currently under review for emergency use authorization having shown 66-85% efficacy in phase 3 clinical trials. The protein subunit NVX-CoV2373 vaccine from Novavax in the US and the inactivated SARS-CoV-2 CorovaVac vaccine from Cansino Biologics in China are expected to complete phase III clinical trials and report efficacy results by late Spring of this year.
AK: How do they all compare?
DZC: Most vaccines undergoing clinical trials or having received regulatory authorization for use in the population elicit production of neutralizing antibodies to SARS-CoV-2 spike protein at high levels.
AK: What about safety?
DZC: Vaccines that have progressed or completed phase 3 clinical trials have demonstrated high safety margins for widespread use. They elicit immune responses and high affinity antibodies that block infection, disease development, and severity. All authorized vaccinees are delivered intramuscularly. Vaccine reactogenicity is temporary and symptoms such as pain, headache, fever, and chills as part of the initial immune system response are usually mild and disappear by 48 hrs after vaccination for the vast majority of vaccines so far. The second dose is usually more reactogenic because the immune system ramps up faster from the level of the previous dose. Older individuals tend to be less reactogenic than younger adults with more robust immune systems. There are intrinsic factors affecting vaccine reactogenicity in addition to age, such as gender, societal, psychological, and work related stress, and circadian cycle that is not synchronized to the immune system’s response as can be the case for workers that switch between day and night shifts. Extrinsic factors include inappropriate administration of the vaccine if the needle is too short or the stick not adequate to reach the intramuscular layer of the deltoid muscle. If it is delivered intradermal or subcutaneously under the skin, immune reactions can be much stronger due to differences in anatomy of pain centers and distribution of immune cells in these tissues.
AK: At the rate the US is dispensing the vaccine, how soon do you think we can achieve herd immunity?
DZC: This is difficult to predict. There are too many moving parts in vaccine manufacturing, availability, dispensation logistics, rate of decline in vaccine hesitance, and race against new clades and sub-strains of the virus that may limit the efficacy of current vaccines.
AK: How important is it that we achieve herd immunity?
DZC: Vaccines are the cornerstone of herd immunity. COVID19 can only be tamed through vaccine induced herd immunity. Without such control, the virus will continue to spread and mutate. It has become a very agile human pathogen having already reached even the most remote populations on earth.
AK: Will we need booster shots due to variants?
DZC: This is not yet known. Most likely.
AK: How much more potent are the variants?
DZC: The five variants that are currently of concern spreading out from England, South Africa, Brazil, and as of two days ago in California appear to be more transmissible. One of the two variants in England has a change in a key amino acid of the spike protein that may lead to increased pathogenicity with additional adaptations of this virus strain.
AK: Will virus mutations make the vaccines less effective?
DZC: The South African and Brazil variants appear to reduce efficacy of the Astra Zeneca Vaccine below a tolerable threshold.
AK: If someone receives the vaccine, will they be protected from the variants?
DZC: Yes, if the vaccine neutralizes the variants
AK: How important is it that people still wear their masks and social distance even if they have been vaccinated?
DZC: Very important. The vaccination campaign has just started. It will be months before data of vaccine effectiveness in the general population ie the ability of the vaccine to reduce disease burden and prevent adverse outcomes in vulnerable populations such the elderly and those with comorbidities. This stage is often referred to as Phase IV. Vaccine effectiveness will be monitored for a long time.
AK: Can you receive the vaccine if you have already had covid?
DZC: Yes, vaccination optimizes antibody affinity and anamnestic responses to infection that may wane after natural immunity develops, and ensures the establishment of herd immunity that is critical to prevent the spread and development of new strains of the virus.
AK: Can people switch between doses of the vaccine?
DZC: No, switching doses between vaccines from different manufacturers is not currently recommended.
AK: If someone received the first dose and got covid before the second dose, should they still take the second dose?
DZC: Yes, the second dose augments the production of high levels of neutralizing antibodies that block infection and, furthermore, can facilitate the eradication of infected cells in the host.
AK: How much time can you delay in receiving the second dose?
DZC: Studies to determine whether longer intervals between the first and second dose can be used are either not complete or have not been concluded. Vaccination results in the production of antibodies in one to three weeks after the first dose, which ramp up faster after the second dose. Anamnestic responses, ie the ability of the immune system to develop memory immune cells that will respond in the long term take longer to develop. Memory B cells are stored in the bone marrow and locally in tissues where they can remain for life until needed. If too much time elapses for the second dose in adult vaccination, the memory cells that started to develop after the first dose can be deleted in the absence of adequate antigenic stimulation.
AK: How long does protection last?
DZC: This is not yet known. Early evidence suggests at least 10 months. Based on data from the previous SARS pandemic in 2002-2003, at least 2 years.
AK: Can you infect someone after you’ve received the vaccine?
DZC: Yes, if there is ongoing asymptomatic or known infection when the vaccine was administered or if you are re-infected with a new strain that the vaccine does not cover. Also if the vaccine has 95% efficacy, 1 in 20 individuals may not generate immunity to the virus, can be infected, and continue to spread the virus before herd immunity is established.